GPs in Northern Ireland are “struggling to the point of collapse,” with a new workforce report demanding urgent action to retain staff in primary care.
Ahead of an event in Stormont on Tuesday afternoon, the Royal College of General Practitioners NI (RCGPNI) detailed the key challenges facing staff.
In A Workforce Fit for the Future, the health and social care system in Northern Ireland is described as “over-stretched and crumbling to the point of crisis”.
Several recommendations were made including expanding GP training places and a sustainable funding model.
Short-term measures were for the creation of a practitioner health programme to help the increasing numbers of GPs facing burnout, tackling workload imbalances and more support for practices at risk of collapse.
With increasing demand outstripping supply, GPs are said to be working “past the point of exhaustion and burnout”.
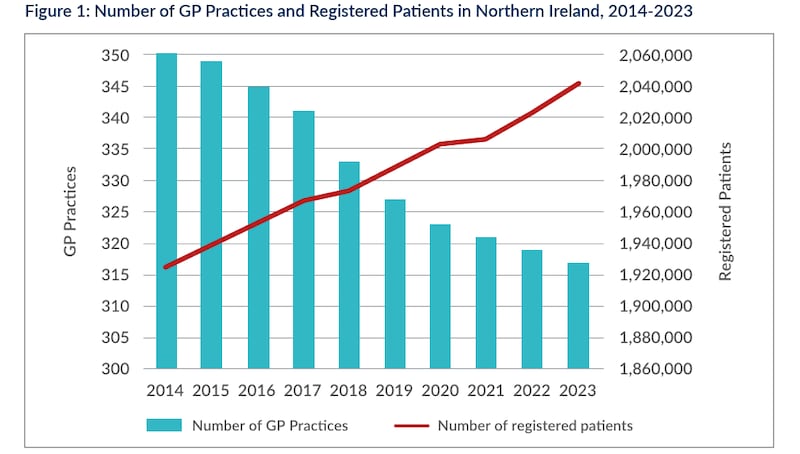
By March 2023, there were 317 active GP services in Northern Ireland – down 33 (9%) since 2014 and two since 2022.
As practices decrease, the average number of registered patients per practice has increased by around 17%, from 5,500 to 6,439 since 2014.
With GPs taking three years to train, the report said retaining existing staff was crucial in the short term – particularly with GPs early in their career who choose to move away from Northern Ireland.
In the past two years, 25 GP practices have handed back their contracts or closed a practice branch site – affecting at least 128,000 patients.
80 practices have also accessed emergency support from the Practice Improvement Crisis Response Team.
RCPGNI staged a number of “Retention Roadshow” events across Northern Ireland in the past year, with around 200 GPs sharing their experiences.
A key theme was that working in general practice was “hugely risky,” both professionally and personally – making doctors consider leaving.
They said addressing the mismatch between increased demand and capacity would improve the quality of their life and work, and ultimately patient care.
Other requests were made for investment in digital technology, creating a state-backed indemnity scheme to reduce the cost of working in Northern Ireland, addressing burnout concerns and core funding.
Negative public narratives “fuelled by some elements of the media” were said to have a serious impact on GP morale – with GPs reporting they felt undervalued and with a poor public understanding of the pressures they were facing.
There was a further perception among many GPs that little help was available to practices until they reached the point of collapse.

Dr Ursula Mason, a GP in Carryduff and chair of RCGPNI, said: “Ultimately, improving the retention of our GP workforce is about keeping general practice afloat and able to provide the safe, effective, and person-centred care which all our patients need and deserve.”
Responding to the report, the Health Minister Robin Swann said that despite serious budgetary issue, he was committed to attracting and recruiting new GPs and retaining experienced doctors.
Since returning as health minister, he said his immediate priority had been to progress the 2023/24 Doctors and Dentists Review Bodies recommendations - recently approving a 6% funding uplift for GPs and their staff.
Annual GP training places have increased from 65 in 2015/16 to the current level of 121, an increase of 86%.
The Department of Health’s Attract, Recruit and Retain Scheme has tried to help practices in hard to recruit areas, while initiatives to support the existing GP workforce has included the introduction of Multi-disciplinary Teams and new roles like Advanced Nurse Practitioners, additional General Practice Nurses and General Practice Pharmacists.
With the incoming 2024/25 budget expected to “remain very challenging,” he said “the main focus will therefore need to be on preserving and protecting existing services, with all the limitations that they currently have”.
“The department is working with GPs to help General Practice to deliver, to grow and to be in the vanguard of how we transform health and social care for our population and for our workforce.”









