Comedian Adam Kay was asked if he was pregnant when he asked to go part-time while working as an NHS doctor.
Both Kay and fellow comedian Harry Hill said that a “get on with it” culture in the NHS drove them away from their jobs as doctors.
While Kay said that he imagines the situation in the NHS has improved since he left a decade ago, Hill said former colleagues who still work in the service have “run out of goodwill.”
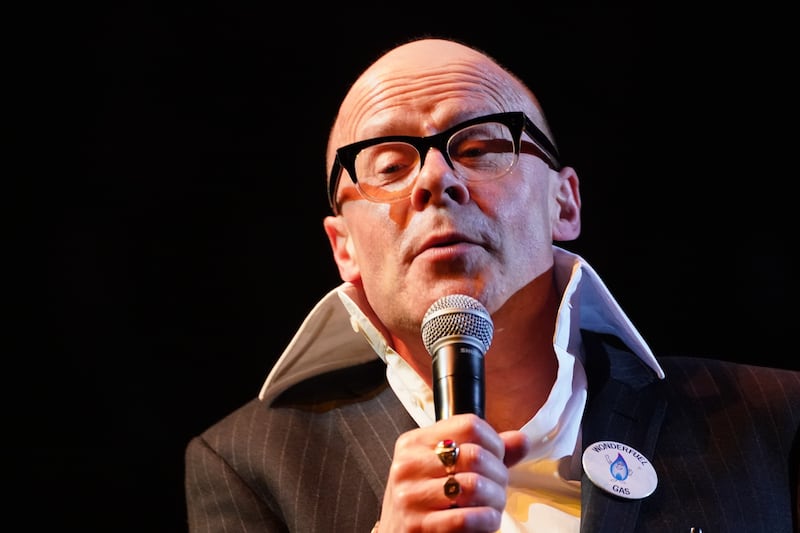
Hill said that he may have remained in the service if “someone had once asked me: ‘How are you getting on’?”
The comedians, along with campaigner and medic Dr Phil Hammond, have been helping academics at the University of Bath and the Royal College of Emergency Medicine who have published a paper on staff retention in the NHS.
Speaking to academics, Kay said: “If I was working in a place where they said ‘do you want a bit of time out? Or do you want a bit of time away from labour ward? Or would you like to be supernumerary for a couple of weeks’ – so you’re a spare pair of hands but the buck isn’t resting just with me – I might have taken up one of those, potentially the last one because that way I wouldn’t have to admit too loudly that I was struggling so badly but it would ease me back into it.”
He added: “I asked to go part-time because I thought maybe that would be a way through just to get to the end of my training and I was asked ‘are you pregnant?’, which is the only way they could see that someone might need to be less than full time.
“I suspect that’s totally different now, I think they’d bite a trainee’s hand off to remain in hospital if there is a choice between part-time or no-time.
“Any of those aspects of support would have helped, even knowing I was in an environment where you were allowed to struggle would help.”
He described a “culture whereby it’s a badge of honour to work as hard as possible, to never say anything is the matter, to constantly plough on ‘you’re a bloody doctor, you bloody get on with it, stiff upper lip, stiff drink, on you go’.”
Kay added: “When you do have a problem, it’s very difficult to actually go and get help.
“Only on one occasion during my time as a doctor did I go and see someone and say I was struggling. I went to see one of the bosses and said I think I might need to step away from this particular clinical scenario for a while, rather than saying no they said: ‘really?’ which I thought was worse because that was belittling my experience.”
Meanwhile Hill said that friends who remain in the health service have told him that the Government “have lost the goodwill of doctors and the (service) has always been run on the goodwill of the people who work in the health service”.
Asked if there was one thing that would have kept him in the NHS, Hill replied: “If someone had once asked me: ‘How are you getting on?’”
He continued: “What I was surprised at and what pushed me over the edge in the sense of me deciding I would jack it in, was the way that we were treated.
“Medical staff were very cold and uninterested. No-one was interested in us as people.
“The consultants really (had an attitude of) ‘we had to do it, get on with it’.
“In fact they hadn’t had to do it, the consultants we worked with they probably qualified in the 60s and there wasn’t the amount of work because there just wasn’t same the number of tests and treatment. Really it was that attitude: ‘get on with it’.”
Dr Hammond said that working in the health service was “unremittingly knackering” and “I don’t think the job is going to get any less stressful”.
The comments were made to academics writing a new paper on staff retention in emergency care.
The article, which has been published in the Emergency Medicine Journal, saw academics interview 33 frontline health service workers about their experience working in health service.
People commonly spoke about a “culture of blame” and workers said that the “toxic” culture had a marked effect on their wellbeing, the authors wrote.
Many described “untenable working environments” with “parallels drawn between being at war and working on the NHS front line”.
One nurse said: “There is the jollying everybody along, being the redcoat on the shift, cheering everybody up, saying everything is going to be okay, but feeling like you’re just rearranging the deckchairs on the Titanic.”
Lead author Dr Jo Daniels, from the University of Bath, said: “Our study asked what more could be done to improve the current challenges of staff retention.
“A common thread that emerged across our interviews was the critical importance of leadership in hospitals.”
Dr Adrian Boyle, president of the Royal College of Emergency Medicine, added: “The NHS must get better at caring for its workforce – its people are its greatest asset, and everything must be done to ensure their welfare.”
A spokesperson for NHS England said: “The NHS is committed to retaining its people, which is why earlier this year we launched the first ever NHS Long Term Workforce Plan that sets out measures to improve culture, leadership and wellbeing and ensure up to 130,000 fewer staff leave the health service over the next 15 years.
“A major new retention programme is already being expanded across the country with data showing the equivalent of 14,000 fewer staff left the NHS in the year to August 2023 compared to the year before, thanks to measures such as more flexible working, clinical support to help menopausal women at work, and HR ‘stay advocates’ who find ways to keep staff considering leaving.”



